Hello, and welcome to Part 3 of my “Why Does My Eye Doctor…” series!
Today we’ll be discussing the importance of the dreaded “eye puff” test.
Ready? Let’s get started with a quick lesson on ocular anatomy!
Ocular Anatomy
Okay, so before we can really discuss the ins and outs of the “air puff” test, it’s important to know a little bit of anatomy.
I think this picture will do!
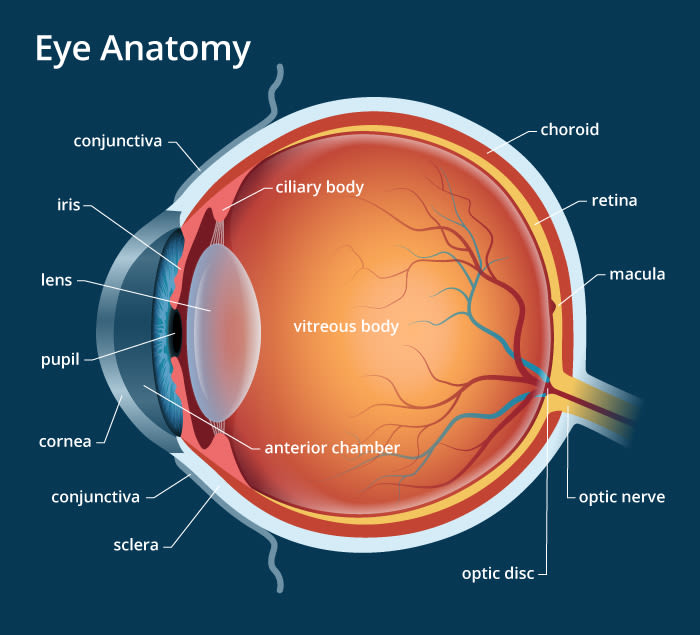
So, where we’re focusing in this picture is the big open space between the clear front surface (the cornea) and the colored part of the eye (the iris). This space is called the anterior chamber (anterior = front). This chamber – or big space – is filled with a fluid called aqueous humor (aqueous = watery, humor = substance within the body).
Keep looking at the picture. You should notice that the cornea and the iris come together at an angle. This angle is called the anterior chamber angle (makes sense, right?). Cells within the angle make the aqueous.
Within this angle, and unfortunately not pictured here, there is another structure, called the trabecular meshwork. It’s really just like a fancy drainage system composed in a net/mesh-like format to allow the aqueous to flow out of the eye.
The goal? Making the amount of aqueous that flows out of the eye essentially equal to the amount of aqueous produced by the eye so that the pressure remains the same.
What is Tonometry?
Okay, so now that we know a little bit about the anatomy of the eye, and so what causes pressure – how do we measure it?
That’s where tonometry comes in.
By definition, tonometry is the measure of the fluid pressure inside the eye. In this, an external force is applied to the eye until the pressure of the external force equals the pressure of the internal force (as determined by slight flattening of the cornea – don’t worry, it’s not dangerous).
There are a few different mechanisms by which this pressure can be assessed.
Non-contact Tonometry
Aka the “puff of air” test.
In this test, nothing really touches your eye (except a little bit of air), therefore it’s non-contact. The air comes out at a certain pressure, that increases until the specified corneal flattening is achieved. The air is then shut off, and the pressure reading provided.
This test isn’t always the most accurate – it tends to overestimate low pressures and underestimate high pressures. That’s why it’s important to get at least 3 readings to provide an average pressure.
Contact Tonometry
As could be expected, in contact tonometry something actually touches your eye (though what it is depends on which specific test is used). As before, this instrument puts pressure on the eye from the outside until that small amount of corneal flattening occurs.
Why Do We Need It?
Most people have probably heard that we check pressure in the eyes as a test for glaucoma.
It’s 100% true.
Glaucoma is a disease in which the internal pressure of the eye is too great for the eye, causing compression of the retinal nerve fibers at the optic nerve. Unfortunately, the longer or harder these fibers are compressed, the more likely they are to die, causing vision loss – first in the periphery or outer parts, and eventually moving to the central/inner parts.
To make matters worse, the retina has no pain fibers – in other words, there’s no pain when the tissue is dying – and since it starts on the outside of your vision, even the vision loss takes time to be noticed. For this reason, glaucoma is considered the silent blinder – there generally are no symptoms.
And, since the retina is brain tissue, once it’s gone, it cannot be replaced.
For this reason, it’s important to have your eyes examined – and their pressures checked – regularly.
Are There Other Options?
In short, yes. There are multiple instruments that can be used to check the internal pressure of the eyes. However, not all offices have all options. The primary ones are:
Non-contact/Puff of Air: Considering this one of the only non-invasive procedures, you’d think it’d be everyone’s favorite. Apparently it’s not.
Goldmann: This is the gold standard, or most accurate, way of measuring eye pressures. I typically use this one in patients that I already know have glaucoma, in patients that I suspect may have glaucoma and am watching closely, or in patients where one of the other tests gave an unexpected reading. Yes, it touches your eye. Don’t worry – your eye is numb for this test. You may feel a bit of pressure, but it won’t be painful.
Tonopen: This was my go-to at the in-patient rehab hospital that I worked at. It tends to underestimate very high pressures, but it works well because it requires very little patient cooperation.
iCare: This one is probably my absolute favorite, because it doesn’t require a numbing drop, and is the most non-invasive of all the procedures (in my opinion). It may tickle your eyelashes a bit, but that’s literally as bad as it gets! Unfortunately, it’s again not as accurate, so if I get unusual readings, I then switch over to Goldmann (if possible considering patient age and ability).
Ocular Response Analyzer: This is (as far as I’m aware anyway) the newest technology when it comes to looking at eye pressures. Similarly to the well known “puff of air” test, it uses air to determine pressures, while concurrently measuring corneal elasticity, or hysteresis. This is another measure of corneal integrity that can provide valuable information when monitoring for glaucoma.
If you have any questions or comments, please contact me! If you’ve enjoyed this article, please subscribe, or like my page on Facebook!