Astigmatism
What is astigmatism?
- *Insert football analogy here*
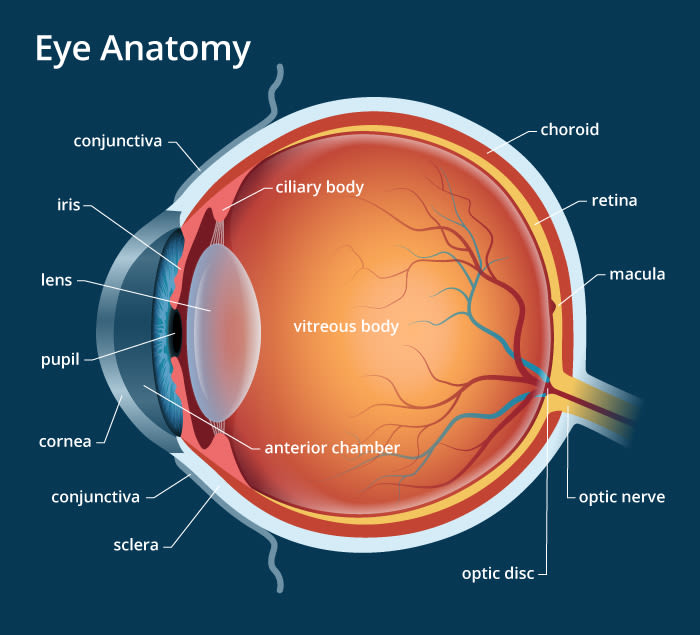
- Just kidding. Your eye really isn’t shaped like a football in astigmatism. Rather, astigmatism occurs when there is more than one power in either the cornea or the lens, as a result of different amounts of curvature. These differences in curvature are generally located 90 degrees away from each other.
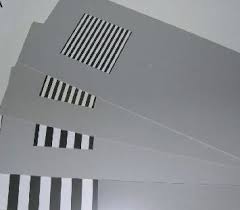
- Here’s a picture to try to help explain:
- In this picture, the red is the steeper, or more curved part (think tennis ball). The blue is the flatter, or less curved part (think bowling ball).

- Because there are different powers, the light focuses in two different spots in relation to the retina, with one closer (either in front of or behind) to the retina, and the other further (so, more in front or more behind) the retina.
Why do we need lenses?
- The goal of lenses in the case of astigmatism is the same as the goal of lenses in hyperopia and myopia – to put a clear image on the retina.
- However, since there are two powers in the eye, there are also two powers in the lens with the goal of putting both images on the retina.
- Some people are lucky and have the perfect split in the two powers that a relatively clear image falls on the retina without glasses. In these cases, wearing lenses may make the image slightly better, but glasses aren’t a requirement.
Who gets astigmatism?
- Refractive errors in general are thought to be inherited. Astigmatism is no different. If you have a history of family members with significant astigmatism, you’re more likely to have it too.
- Astigmatism can occur in both near-sighted and far-sighted individuals.
- Most infants are born with a moderate amount of astigmatism that tends to decrease with age (along with their hyperopia). The concern comes when the level of astigmatism is outside normal ranges, and fails to decrease with age.
- Astigmatism may occur after trauma to the eye that causes corneal scarring.
- Patients of African-American or Hispanic ethnicity are more likely to have higher levels of astigmatism.
When should I suspect astigmatism?
- Some signs of having astigmatism are:
- Squinting, either at distance or near (or both)
- Complaints of glare or halos around lights
Are there any complications with having astigmatism?
-
If someone has a high amount of astigmatism from a young age that is not treated, they may develop amblyopia, or potentially permanently reduced vision as a result of not having a clear image on the retina.
Can astigmatism be treated?
- Most often, patients are prescribed glasses or contacts to improve vision.
- Refractive surgery can also be used to change the power of the eye.
If you have any questions or comments, please contact me! If you’ve enjoyed this article, please subscribe, or like my page on Facebook!