Welcome back to my “Why Does My Eye Doctor…” series!
Have you ever wondered, “Why does my optometrist care so much about my medical history? That has nothing to do with my eyes!!”
If so, you’re not alone. It can definitely seem weird being asked (or being the doctor and asking) about general medical history while at the eye doctor, but I promise it isn’t just to be nose-y!
Believe it or not, your ocular health is closely related to your systemic health, and your eyes are often one of the first places to show systemic disease!
Sound crazy? Let’s take a look at four (relatively) common conditions that can be seen in your eyes!
Diabetes
- Diabetes is a disease that affects the small blood vessels in your body. (Okay, it affects larger vessels too, but for the sake of the eye, we’re focusing on the smaller ones.)
- In the eyes (specifically the retina), this can cause bleeding, or hemorrhages, as well as leakage of other materials from the blood vessels. If this bleeding or leakage happens to be around the macula, or part of the eye responsible for your best vision, it can cause swelling that then distorts your vision.
- Fluctuations in blood sugar levels can also affect your vision, as they cause changes within the lens of your eye. If you notice frequent changes in vision, it may be a sign of diabetes.
Hypertension
- High blood pressure is, once again, a disease of the small blood vessels in your body.
- The retinal disease (retinopathy) associated with hypertension occurs in 3 main stages.
- Vasoconstrictive: This is a fancy way of saying that the blood vessels constrict in response to the increase in blood pressure. The goal of the constriction (which is automatically controlled) is to decrease the amount of blood flow so that the normal vessel system of the retina isn’t overwhelmed. This early stage is seen in the eye as arteriolar narrowing. *I would include a picture, but it can be pretty hard to appreciate*
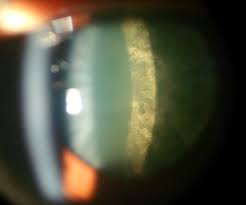
- Sclerotic: The term sclerosis simply means hardening. The constriction of the blood vessels in the vasoconstrictive phase occurs via a muscular layer in the arteries. Like any muscle that is frequently used, over time, this muscular layer gets bigger, making the arteries harder. As the arteries harden and become heavier, they compress the underlying veins. This causes a characteristic appearance of blood vessel “nicking” as seen below, where the vein becomes diminished upon artery crossing.

- Exudative: Once enough compression has occurred in the sclerotic phase, blood, fats, and additional components begin to leak out of the vessels, signaling a transition to the exudative phase. In this stage, hemorrhages (areas of bleeding), exudates (hard, fatty deposits), and edema (swelling from leaking fluid) are common. As blood vessel compression also reduces blood flow (stasis), clots are more likely to form, occluding, or blocking the vessel. Without proper blood flow, ischemia (literally lack of blood flow) occurs, causing subsequent damage to affected tissues.

Thyroid Disease
- First things first: thyroid problems can come in two forms – overactive (hyperthyroid) or underactive (hypothyroid).
- Both versions can be caused by autoimmune states. The one most commonly associated with hyperthyroidism is Grave’s Disease, while the one most commonly associated with hypothyroidism is Hashimoto’s Disease.
- In addition to systemic manifestations, both hyper and hypothyroidism may present in the eyes. Possible symptoms include:
- Redness
- Dryness and irritation
- Swelling around the eyes
- Protrusion of the eyes
- Pain with eye movement
- Inability to fully close the eyes
- Double vision
- Loss of vision
- These symptoms may occur in existing cases of autoimmune related thyroid disease, or may be among the first presentations of the condition. If your doctor suspects thyroid disease secondary to ocular presentations, they will likely ask a number of systemic questions that seem totally unrelated such as:
- Unintentional/unexplained weight gain or weight loss
- Sensitivity to heat or cold
- Changes in energy levels (either very high or very low)
- Changes in mood (such as being highly irritable or more depressed)
- Changes in bowel movements
- Changes in menstruation
- If your doctor asks these seemingly off the wall questions, don’t freak out! They’re trying to narrow down the potential causes of your symptoms so that they can send you to the right place to get the right diagnosis!
Multiple Sclerosis
- While we’re on the topic of autoimmune diseases, it’s important to discuss Multiple Sclerosis.
- In this condition, antibodies attack the myelin (protective coating) that surrounds nerves in your central nervous system (brain and spine). This causes demyelination (literally, loss of myelin) around the nerve, which impedes transfer of the signal from the brain to its intended recipient.
- One of the more common, and often early, presentations of multiple sclerosis is optic neuritis, or inflammation of the optic nerve.
- Optic neuritis generally presents as mild-moderate vision loss in a single eye that comes on suddenly and may worsen for around 2 weeks, after which symptoms begin to improve. Colors may seem less vibrant out of this eye, and there is often pain with eye movement.
- As with any sudden decrease/loss of vision, it is important to see an eye doctor with these symptoms.
- Looking in the back of your eye, the doctor will often see nothing out of the ordinary. This is because the inflammation is behind your eye (retrobulbar).
- Your doctor should order an MRI, with and without contrast, to aid in diagnosis. The results of this test provide important information regarding future prognosis as:
- 1/4 people with no other lesions on MRI have a diagnosis of Multiple Sclerosis within 15 years
- 2/4 people with optic neuritis are diagnosed with Multiple Sclerosis within 15 years
- 3/4 people with another characteristic MRI lesion are diagnosed with Multiple Sclerosis in 15 years
- As before, your eye doctor may ask about other systemic symptoms as well, such as:
- Fatigue
- Dizziness
- Numbness/Weakness
- Tremor
- Please don’t avoid the questions, or think your eye doctor is practicing outside his or her scope! Believe it or not, as optometrists, we are trained to know the symptoms of systemic diseases that may present in your eye.
If you learned something from this post, please share it with a friend or family member! If you liked it, please subscribe, or like my page on Facebook! And as always, if you have any questions or comments, please contact me – I’d love to hear from you!
This is Part 4 of my “Why Does My Eye Doctor” series – click the links below to check out Parts 1-3!
Part 1 – Dilation
Part 2 – Which is Better, 1 or 2?
Part 3 – Air Puff Test